Have a Question?
Sleep Health in Seniors: Common Disorders, Sleep Apnea, and Strategies for Better Rest

You spend a third of your life asleep. Or at least, you’re supposed to. For many older Australians, sleep has become something they chase rather than something they get. Eight hours turns into six, then five, then fragmented stretches punctuated by trips to the bathroom, racing thoughts, or gasping for air.
It’s easy to dismiss poor sleep as just part of ageing. But sleep disorders aren’t inevitable. They’re often treatable, sometimes preventable, and almost always worth taking seriously. Because sleep affects everything: your immune function, your memory, your mood, your heart health, even your risk of falls.
This blog covers the sleep disorders most commonly affecting seniors, with a particular focus on sleep apnea: a condition affecting about 5% of Australians, often undiagnosed and quietly dangerous. You’ll learn what causes these disorders, how to recognise the warning signs, and what you can do to reclaim restful, restorative sleep.
Why Sleep Matters for Seniors
Quality sleep isn’t a luxury. It’s a biological necessity. For seniors, adequate sleep:
- Supports immune function: Helping your body fight infections and recover from illness
- Regulates mood: Reducing risk of depression and anxiety
- Enhances memory consolidation: Supporting cognitive function and reducing dementia risk
- Promotes cardiovascular health: Lowering blood pressure and reducing heart disease risk
- Improves physical coordination: Reducing fall risk and supporting mobility
Unfortunately, many seniors experience disruptions in their sleep patterns due to
age-related changes in circadian rhythms, underlying health conditions, medication side effects and lifestyle factors. Understanding these disruptions is the first step toward addressing them.
Common Sleep Disorders in Seniors
1. Insomnia
Insomnia is characterised by difficulty falling asleep, staying asleep or waking up too early and being unable to return to sleep. Seniors may experience insomnia due to stress, anxiety, depression, chronic pain or medical conditions such as arthritis or heart disease. Persistent insomnia can lead to daytime fatigue, mood disturbances and reduced quality of life.
2. Sleep Apnea
Sleep apnea is characterised by repetitive episodes of interrupted breathing during sleep, often accompanied by loud snoring and daytime fatigue. Seniors with sleep apnea may be at increased risk of cardiovascular problems, stroke and cognitive impairment. We’ll explore this condition in detail in the next section.
3. Restless Legs Syndrome (RLS)
RLS is a neurological disorder characterised by uncomfortable sensations in the legs and an uncontrollable urge to move them, often occurring at night and interfering with sleep. Seniors with RLS may experience difficulty falling asleep and disrupted sleep patterns, leading to significant daytime fatigue.
4. Periodic Limb Movement Disorder (PLMD)
PLMD is characterised by repetitive leg movements during sleep, which can disrupt sleep and lead to daytime fatigue. Seniors with PLMD may experience restless sleep and involuntary leg twitching or jerking movements, often without being aware of them.
5. Circadian Rhythm Disorders
Circadian rhythm disorders, such as advanced sleep phase syndrome and delayed sleep phase syndrome, involve disruptions in the body’s internal clock. These can lead to difficulties falling asleep and waking up at appropriate times, affecting sleep-wake cycles and contributing to insomnia and daytime sleepiness.
Understanding Sleep Apnea: The Silent Sleep Disruptor
Sleep apnea is one of the most serious and commonly undiagnosed sleep disorders affecting seniors. These pauses in breathing, known as apneas, can last for seconds to minutes and may occur multiple times throughout the night, severely disrupting sleep quality and oxygen delivery to vital organs.
Types of Sleep Apnea
Obstructive Sleep Apnea (OSA)
This is the most common form of sleep apnea and occurs when the muscles in the throat relax excessively during sleep, causing the airway to become blocked or narrowed. OSA is typically caused by anatomical factors such as excess weight, enlarged tonsils, a narrow airway or structural abnormalities in the throat or jaw.
Central Sleep Apnea (CSA)
Central sleep apnea occurs when the brain fails to send the appropriate signals to the muscles that control breathing during sleep. Unlike OSA, there is no physical obstruction of the airway. CSA is often associated with underlying medical conditions such as heart failure, stroke, brainstem disorders or the use of certain medications.
Mixed Sleep Apnea
Mixed sleep apnea is a combination of both obstructive and central sleep apnea, with characteristics of both types present. It may result from a combination of anatomical factors and underlying medical conditions.
Recognising Sleep Apnea: Signs and Symptoms
Common symptoms of sleep apnea include:
- Loud snoring: Often reported by bed partners
- Pauses in breathing during sleep: Witnessed by others
- Gasping or choking sensations: Jolting awake struggling for air
- Excessive daytime sleepiness: Despite spending adequate time in bed
- Morning headaches: Often severe upon waking
- Difficulty concentrating: Memory problems and mental fog
- Irritability or mood changes: Depression or anxiety
- Frequent night-time urination: Nocturia
Important: Not everyone with sleep apnea experiences all of these symptoms, and severity can vary from person to person. Some people aren’t even aware they have the condition.
The Dangers of Uncontrolled Sleep Apnea
Sleep apnea affects about 5% of Australians and is particularly common among men over 30, with 1 in 4 affected. This is about three times more than women in the same age group. Left untreated, sleep apnea can have serious consequences:
- Cardiovascular disease: Increased risk of high blood pressure, heart attack, stroke and irregular heartbeat
- Type 2 diabetes: Sleep apnea is linked to insulin resistance
- Cognitive decline: Increased risk of dementia and memory problems
- Depression and anxiety: Disrupted sleep significantly impacts mental health
- Unexplained fatigue: Chronic tiredness affecting daily functioning
- Increased fall risk: Daytime drowsiness and impaired coordination
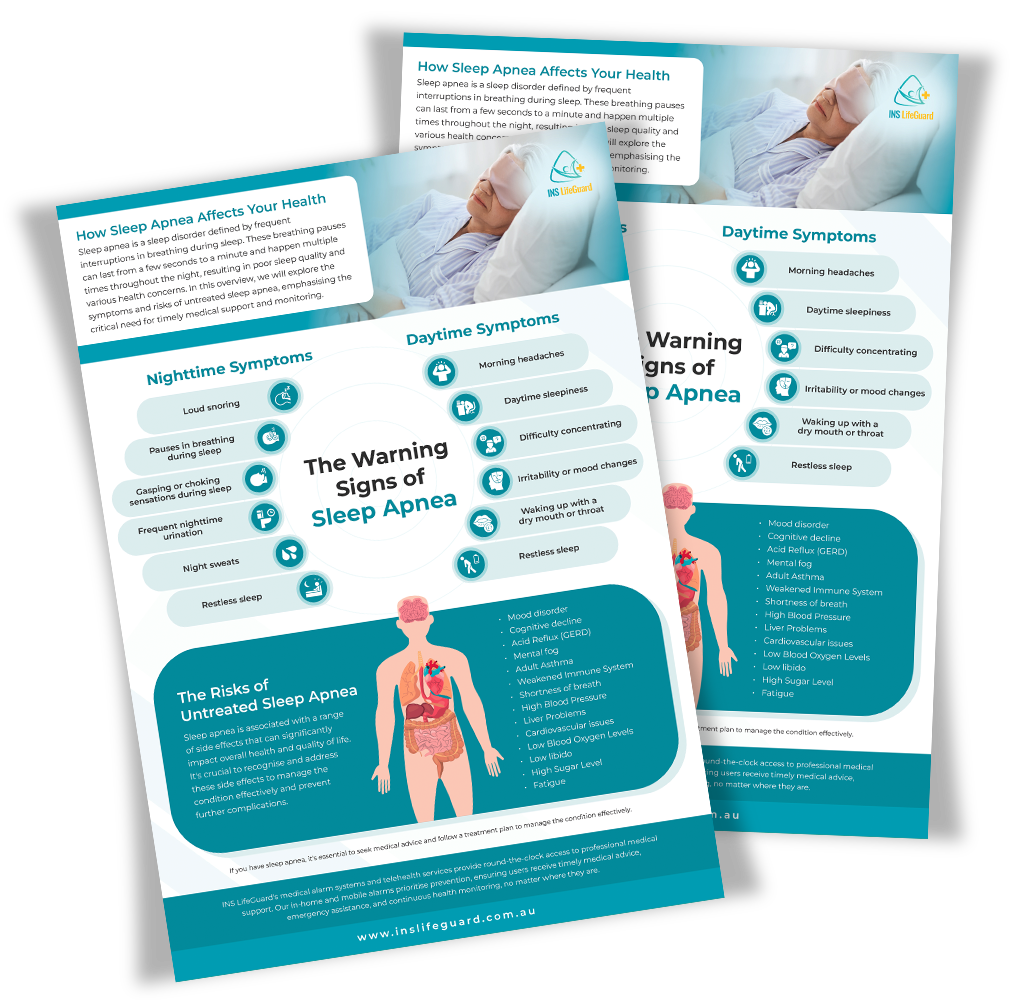
Download Your Free Sleep Apnea Guide
Learn the symptoms and dangers of uncontrolled sleep apnea. This comprehensive guide helps you recognise warning signs and understand the risks so you can take action.
Treatment Options for Sleep Apnea
The good news is that sleep apnea is treatable. Treatment depends on the type and severity of the condition:
Lifestyle Modifications
Making lifestyle changes can significantly reduce sleep apnea symptoms:
Losing weight if overweight or obese
Quitting smoking
Avoiding alcohol and sedatives before bedtime
Sleeping on your side rather than your back
Continuous Positive Airway Pressure (CPAP) Therapy
CPAP therapy is the most common treatment for obstructive sleep apnea. It involves wearing a mask connected to a machine that delivers a continuous flow of air to keep the airway open during sleep. Whilst it takes some adjustment, CPAP therapy is highly effective for most people.
Oral Appliances
Oral appliances, such as mandibular advancement devices, can help keep the airway open by repositioning the jaw and tongue during sleep. These devices are custom-made by a dentist and may be recommended for mild to moderate cases of sleep apnea.
Surgery
In some cases, surgery may be recommended to remove excess tissue from the throat, reposition the jaw or correct structural abnormalities that contribute to sleep apnea. Surgical options are typically considered when other treatments haven’t been effective.
Strategies for Better Sleep Hygiene
Regardless of whether you have a diagnosed sleep disorder, practising good sleep hygiene can significantly improve sleep quality:
1. Establish a Consistent Sleep Schedule
Go to bed and wake up at the same time every day, even on weekends. This helps regulate your body’s internal clock and improves sleep quality over time.
2. Create a Relaxing Bedtime Routine
Engage in calming activities before bedtime, such as reading, listening to soothing music or practising relaxation techniques. This signals to your body that it’s time to wind down.
3. Maintain a Comfortable Sleep Environment
Keep your bedroom cool, dark and quiet. Invest in a comfortable mattress and pillows. Consider using blackout curtains, white noise machines or earplugs if needed.
4. Limit Stimulants and Alcohol
Avoid consuming caffeine, nicotine and alcohol close to bedtime. These substances can interfere with sleep quality and exacerbate sleep disorders.
5. Stay Active During the Day
Regular physical activity can promote better sleep quality and help you fall asleep more easily. However, avoid vigorous exercise close to bedtime, as it can have a stimulating effect.
When to Seek Professional Help
It’s essential to seek medical attention if you experience:
- Persistent difficulty falling or staying asleep for more than a few weeks
- Loud snoring accompanied by breathing pauses during sleep
- Excessive daytime sleepiness that interferes with daily activities
- Symptoms of depression or anxiety related to poor sleep
- Any sleep-related symptoms that significantly impact your quality of life
Early diagnosis and treatment of sleep disorders can prevent serious health complications and dramatically improve quality of life. Don’t dismiss poor sleep as just part of ageing—seek help from a qualified healthcare provider.
How INS LifeGuard Supports Sleep Health and Safety
Whilst sleep disorders require medical treatment, INS LifeGuard provides comprehensive support for the safety challenges that often accompany poor sleep in seniors:
Fall Detection and Prevention
Daytime drowsiness from sleep disorders increases fall risk. Our INS LifeGuardian® app with Apple Watch or compatible wearables provides automatic fall detection, immediately alerting our 24/7 nurse-led response team if a fall is detected.
24/7 Nurse Support
Whether you’re experiencing concerning symptoms at 2am or need reassurance about sleep-related health changes, our qualified nurses are available around the clock. They can provide clinical guidance, answer questions and escalate to emergency services if needed.
Health Monitoring
Track vital signs including heart rate, oxygen saturation and activity patterns. Changes in these metrics can indicate sleep disorder complications or other health issues requiring attention.
Medication Reminders
For those managing sleep disorders with medication or CPAP therapy, customisable reminders help provide treatment adherence, improving outcomes and sleep quality.
Night-Time Safety
For seniors who experience frequent nighttime awakenings or bathroom trips, having immediate access to emergency support provides peace of mind. A simple press of a button connects you to professional help, reducing anxiety that can further disrupt sleep.
Reclaiming Restful Sleep
Sleep disorders aren’t something you just have to live with. They’re medical conditions with real consequences and real solutions. Whether it’s insomnia keeping you awake, sleep apnea stealing your oxygen, or restless legs preventing rest, treatment exists.
The first step is recognising that your sleep matters. The second is seeking help. And the third is building safety systems that support you whilst you work towards better rest. These are systems that catch you if you fall, monitor your health between appointments, and connect you to qualified nurses whenever uncertainty strikes at 3am.
Because everyone deserves to wake up feeling rested, not just relieved they made it through another night. Call us on Call
1800 636 226 or
browse through our website to learn how INS LifeGuard can support your health and safety as you work towards better sleep.

About
INS LifeGuard is the only 24/7 nurse on-call personal and medical monitoring in Australia. We provide monitoring technology for both in the home and on the go and can also monitor other provider's equipment. Our services are suitable for anyone wanting support to stay independent such as the elderly, those with medical conditions and disabilities plus enhancing safety and security for lone workers.